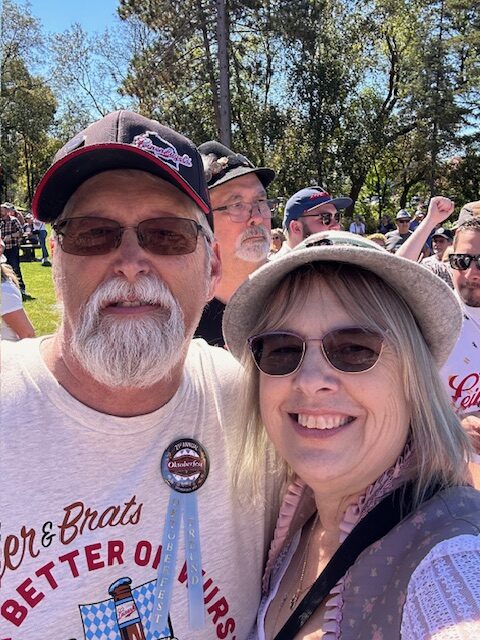
Julie Whyte Pancreatic Cancer Survivor
Julia Brabant, May 2025No One Fights Alone: How Family, Faith & Hope Helped Julie Whyte Reach 4 Years of Pancreatic Cancer Survivorship
When Julie Whyte of Prairie du Chien, Wisconsin, started experiencing trouble breathing and ongoing abdominal pain in her right side, she didn’t initially suspect something serious. Neither did the doctor she sought treatment from when the pain persisted, with the physician telling Julie she had a less than 1% chance of having cancer. Yet, that 1% soon became her reality, with doctors diagnosing her with pancreatic cancer in the winter of 2021. Four years later, Julie continues to defy statistics, and she recently held her first grandchild in her arms; a healthy baby boy who served as a powerful reminder that some odds are meant to be overcome.
Julie’s diagnosis came in early 2021, after a bout with COVID-19 caused breathing issues and landed her in the emergency room. ER doctors administered a D-dimer test, which assesses patients for signs of abnormal blood clotting. Julie’s test results were on the high side, so doctors performed a CT scan with the hope of identifying any blood clots.
While the scan didn’t reveal any clotting, it did show a gallbladder full of gallstones, but her nurse practitioner told her she wouldn’t need to do much about it unless they continued to bother her.
Julie’s pain persisted, proving especially painful on her right side. She went to the chiropractor to see if it would bring her some relief, but it failed to do so, and she continued having severe pain when performing certain movements, like getting in and out of the car or lifting her leg up high.
After a weekend away with family and friends, Julie returned home and saw her pain progress to the point where her husband, Todd, insisted she return to the emergency room in the middle of the night. They lived in a small, rural community, though, and the local ER doctors were unable to perform an ultrasound at that time, leading to another CT scan.
Doctors again told Julie the problem lay in her gallbladder, sending her to a larger facility in Dubuque, Iowa, the next day to have her gallbladder removed. When the gastrointestinal surgeon reviewed Julie’s scans, he spotted a “shadowy area,” noting that he and one of the hospital’s radiologists wanted to take a closer look at the spot in question.
The hospital in Dubuque took out Julie’s gallbladder and put her in touch with physicians at the UW Health | Carbone Cancer Center in Madison, Wisconsin. There, Julie’s doctor scheduled her for an endoscopic ultrasound, but told her she had a less than 1% chance of the shadowy area turning out to be cancer.
Unfortunately, the endoscopic ultrasound revealed that Julie did, in fact, have pancreatic cancer (“I’m an overachiever!” she joked), so things moved quickly after that, with Julie having a video conference call (due to the ongoing COVID-19 pandemic) with an oncologist, surgical oncologist and nutritionist.
While, often, doctors have a patient with pancreatic cancer undergo chemotherapy before having surgery, Julie’s care team thought her cancer cells might be resistant to chemo, so they arranged for her to have a Whipple procedure, an intensive operation used to treat some people with pancreatic cancer, as soon as possible.
Julie had an eight-hour Whipple procedure March 5, 2021, and remained in the hospital for another eight days. About six weeks later, she began having adjuvant chemotherapy, or chemo after surgery, to reduce the risk of the cancer returning. She began taking FOLFIRINOX in mid-April and continued through late October, finding that the chemo treatments proved especially brutal.

It’s been a long haul, chemo was worse than the Whipple
“It’s been a long haul,” she said. “Honestly, chemo was worse than the Whipple.”
While Julie felt lucky not to experience nausea, a common side effect of chemotherapy, she did have considerable fatigue. She also found that her liver enzymes shot up, ending up five times higher than is typical so they removed the irinotecan, one of the drugs in FOLFIRINOX, after her third treatment. Her care team also ended up removing Oxaliplatin from Julie’s lineup after she began experiencing severe neuropathy, another common side effect of chemo treatment.
Follow-up scans revealed that Julie had two lesions in her liver, so her doctors performed an MRI to assess their makeup and severity. It turned out both lesions were cysts, and while she still has both spots, they haven’t changed in the time since.
That said, the impact of treatment continues to shape Julie’s day-to-day life. Health challenges led her to leave her job as a retail merchandiser, but she was able to get long-term disability, giving her one less thing to worry about while continuing her recovery. She also switched places with her husband in 2025, stepping into the role he previously held as a caregiver while he went through some serious health issues of his own.
Despite these challenges, both Julie and Todd had something to smile about – their first grandbaby, William Alan, arrived February 9, bringing new light and purpose into their lives. Moments like these have become even more meaningful in recent years, with Julie noting that her strong support system, including her husband, children, siblings, extended family and friends, played a huge part in helping her navigate ongoing challenges.
Her support network even surprised Julie with several parties, with one taking place before she began chemo and another acknowledging both the end of her chemo treatments and Julie reaching another birthday. At one of those celebrations, Julie’s niece handed out custom T-shirts that read, “In this family, no one fights alone,” a simple phrase that captured the love and strength that have surrounded Julie since the beginning. She also found joy in spending time with her dogs, a Yellow Labrador and a Cavalier King Charles/Cocker Spaniel mix who rarely left her side during treatment. That second dog, her constant companion during the hardest days, passed away just 10 days after Julie completed chemo – as if she’d waited until Julie was safely through the fight before letting go.
These days, Julie still experiences neuropathy in her toes and fingertips, which she treats using alpha-lipoic acid on the advice of one of her nurses. She also eats relatively normally, although she takes CREON to help with digestion.
Julie is also taking steps to build strength in the aftermath of her ordeal, investing in an E-bike for exercise and a vibration plate (sometimes called a “power plate”) to help release toxins and stimulate muscle contractions.
She’s also had time to reflect on the treatment she received from multiple facilities throughout her experience with pancreatic cancer, gaining perspective on what worked well and where there might be room for improvement. While, overall, she had positive experiences with medical professionals, she does wish those treating people with pancreatic cancer would take more time with patients and give deeper, more thorough answers and explanations to patient questions.
For example, Julie found that it was often up to her to ask about blood pressure, which, in her case, had always been normal before her diagnosis but rose sharply in the days and months that followed. She wishes health care professionals would take a more proactive approach to asking about and addressing such questions, rather than relying on patients, many of whom lack medical training, to raise such concerns.
She also hopes that, in the future, medical specialists will communicate more with one another, with, for example, cardiologists and oncologists speaking more frequently to provide more coordinated and comprehensive care. Julie believes increased communications would help ease the burden on patients, and that it may also lead to better outcomes and improved quality of life.

You have to fight for your life; advocate for yourself and find someone to help you advocate for yourself. You have to be on top of it for YOU – and for your family.
“Communication isn’t the greatest sometimes,” she said. “I’d like to hear more, ‘We don’t know, but we can look into it for you.’”
Julie also has some advice for other people navigating similar situations, encouraging people with pancreatic cancer diagnoses to avoid making the common, but inaccurate, assumption that such a diagnosis is a death sentence. She also urges them to track down relevant information about clinical trials and potential treatment options and to turn to those who specialize in their specific issue – for example, if a patient’s tumor has arterial involvement, she encourages them to seek care from specialists who regularly treat these complex cases.
She also advises those fighting pancreatic cancer to find strength through their support systems, whether those include family members, friends, church groups or cancer coalitions or support groups, among other examples. She noted that, in her case, she found it especially beneficial to have her husband force her to eat when she felt like she couldn’t. And while Julie advocates for leaning on others when necessary, she also emphasizes the role each patient plays in his or her journey and survival story.
“You have to fight for your life; advocate for yourself and find someone to help you advocate for yourself,” she said. “You have to be on top of it for YOU – and for your family. My kids said, ‘You’re not going to leave us, Mom,’ and I didn’t.’”
She also highlights the importance of maintaining a positive mindset, both amid treatment and afterward.
“Try to stay as positive as you can,” Julie said. “And don’t let anyone put an expiration date on you – that’s between you and God.”