Main Causes of Chronic Pancreatitis, Risk Factors and Symptoms
On This Page: Chronic Pancreatitis
Jump To Section
Written By Tony Subia
April 12, 2022
About Chronic Pancreatitis
The pancreas, a vital organ nestled in the abdomen, plays a crucial role in both the digestive and endocrine systems of the body. This complex organ is responsible for producing digestive enzymes that aid in breaking down food in the small intestine, as well as hormones like insulin and glucagon that regulate blood sugar levels. Diseases of the pancreas, including acute pancreatitis, chronic pancreatitis, and pancreatic cancer, represent significant challenges in gastroenterology, impacting both the exocrine and endocrine functions of the pancreas. Acute pancreatitis, characterized by sudden inflammation of the pancreas, often resolves itself, but when this inflammation becomes persistent and progressive, it leads to chronic pancreatitis. This condition can evolve into more severe forms, including pancreatic cysts and even pancreatic cancer.
Chronic pancreatitis, often a result of prolonged alcohol use, recurrent gallstones, or autoimmune disorders, can lead to a range of complications such as blockages in the pancreatic duct, formation of cysts and pseudocysts, and severe abdominal pain. These issues not only impair the pancreas’s ability to produce and secrete digestive enzymes but can also lead to malnutrition, weight loss, and digestive abnormalities. In some cases, the inflammation extends to nearby organs like the gallbladder and bile duct, causing additional complications like jaundice. The National Pancreas Foundation and other healthcare organizations emphasize the importance of understanding the risk factors and causes of pancreatic diseases, including hereditary pancreatitis and cystic fibrosis. Early diagnosis through imaging tests, endoscopic ultrasound, CT scans, blood tests, and endoscopic retrograde cholangiopancreatography (ERCP) is crucial for effective pain management and treatment, which may include pancreatic enzyme supplementation for exocrine pancreatic insufficiency (EPI), or even surgical interventions like pancreatectomy in severe cases. This comprehensive approach to pancreatic health underscores the intricate nature of diagnosing and treating diseases of the pancreas, emphasizing the need for personalized healthcare informed by a patient’s family history and specific risk factors.
Chronic Pancreatitis is an extreme, long term inflammation of the pancreas that usually has recurring episodes.
Chronic pancreatitis never heals and gets worse over time eventually leading to permanent, irreversible damage to the pancreas. The pancreas plays a dual role to the body. Its “Exocrine Function” is to produce digestive enzymes. When we eat, it triggers the pancreas to send digestive enzymes to the small intestine to digest the food we eat. That process turns food into nutrients that are sent around the body to provide needed energy to the body’s cells.
The other role the pancreas is its “Endocrine Function” which produces hormones such as insulin that regulate the levels of blood sugar in the bloodstream.
What is Chronic Pancreatitis?
Chronic pancreatitis is a long-standing inflammation of the pancreas that alters its normal structure and functions. It is characterized by the irreversible destruction of the pancreatic tissue, leading to fibrosis and the loss of both exocrine and endocrine functions of the pancreas. This condition is typically marked by a persistent state of pain and a progressive loss in pancreatic function, often leading to malabsorption and diabetes. The inflammation and fibrosis in chronic pancreatitis differ from acute pancreatitis, where the damage is usually temporary and reversible.
In chronic pancreatitis, the damage to the pancreas is progressive, meaning that it worsens over time. This progression often results in the creation of calcifications within the pancreas, as well as cysts and pseudo-cysts. These structural changes can cause severe abdominal pain and impair the pancreas’s ability to produce digestive enzymes and hormones, including insulin. The chronic nature of the disease often leads to a reduced quality of life due to constant pain and nutritional deficiencies.
Chronic Pancreatitis is an extreme, long term inflammation of the pancreas that usually has recurring episodes. Chronic pancreatitis never heals and gets worse over time eventually leading to permanent, irreversible damage to the pancreas. The pancreas plays a dual role to the body. Its “Exocrine Function” is to produce digestive enzymes. When we eat, it triggers the pancreas to send digestive enzymes to the small intestine to digest the food we eat. That process turns food into nutrients that are sent around the body to provide needed energy to the body’s cells.
The other role the pancreas is its “Endocrine Function” which produces hormones such as insulin that regulate the levels of blood sugar in the bloodstream.
What Causes Chronic Pancreatitis?
Chronic pancreatitis is commonly caused by prolonged alcohol abuse, accounting for a significant percentage of cases. The exact mechanism by which alcohol induces chronic pancreatitis is complex and involves direct toxic effects on pancreatic cells, oxidative stress, and the formation of protein plugs within the ducts. Other causes include genetic disorders like cystic fibrosis, autoimmune conditions, and recurrent acute pancreatitis, which can lead to chronic changes over time.
Sometimes, the cause of chronic pancreatitis is idiopathic, meaning it occurs without a known reason. Certain hereditary conditions can predispose individuals to the disease, and smoking is also a significant risk factor. Pancreatic duct obstructions, due to stones or tumors, can lead to chronic pancreatitis by causing repeated episodes of inflammation. Less commonly, medications and certain metabolic disorders are implicated. Understanding the cause is crucial for effective management and treatment of chronic pancreatitis.
Chronic pancreatitis is caused by a continuing long term inflammation which develops slowly over time and is most triggered by poor lifestyle factors which includes heavy abuse of alcohol and and heavy, longstanding use of tobacco. However, those are not always the cause of chronic pancreatitis. Other less common causes of chronic pancreatitis that places stress on the pancreas includes the following:
> Autoimmune conditions when the the body’s own immune system attacks itself.
> Genetic mutations often caused by cystic fibrosis. This can be hereditary.
> Blocked pancreatic ducts or the common bile duct often by gall stones.
> Familial pancreatitis when 2 or more immediate family members with a history of pancreatitis.
> Elevated levels of triglycerides.
> Multiple episodes of Acute Pancreatitis.
> Sometimes the cause pf chronic pancreatitis is unknown.
What Happens If The Pancreas Does Not Produce Adequate Levels of Digestive Enzymes?
When the pancreas fails to produce adequate levels of digestive enzymes, a condition known as pancreatic exocrine insufficiency (PEI) occurs. This leads to the malabsorption of fats, proteins, and carbohydrates, causing nutrient deficiencies and weight loss. Without these enzymes, the body cannot break down and absorb nutrients effectively, resulting in steatorrhea – the excretion of undigested fats in the stool, which is often foul-smelling and greasy.
PEI also leads to deficiencies in fat-soluble vitamins (A, D, E, and K) due to their impaired absorption. This can result in various symptoms, including vision problems, bone pain, coagulopathy, and immune system impairments. Patients with chronic pancreatitis often experience chronic abdominal pain, which can be debilitating. The malabsorption of nutrients also leads to muscle wasting and weakness, further impacting the quality of life.
If the digestive function of the pancreas does not perform properly, it will either not produce digestive enzymes at all or will produced a diminished supply. In those cases the small intestine will not properly digest food to provide the necessary nutrients the body requires.
People stricken with chronic pancreatitis which is a serious inflammation of the pancreas can experience unhealthy levels of blood sugar (glucose) in the bloodstream which can lead to type 2 diabetes, weakened bones, vision problems. Most people with chronic pancreatitis have difficulty gaining or maintaining weight and will have some persistent pain and can become debilitating
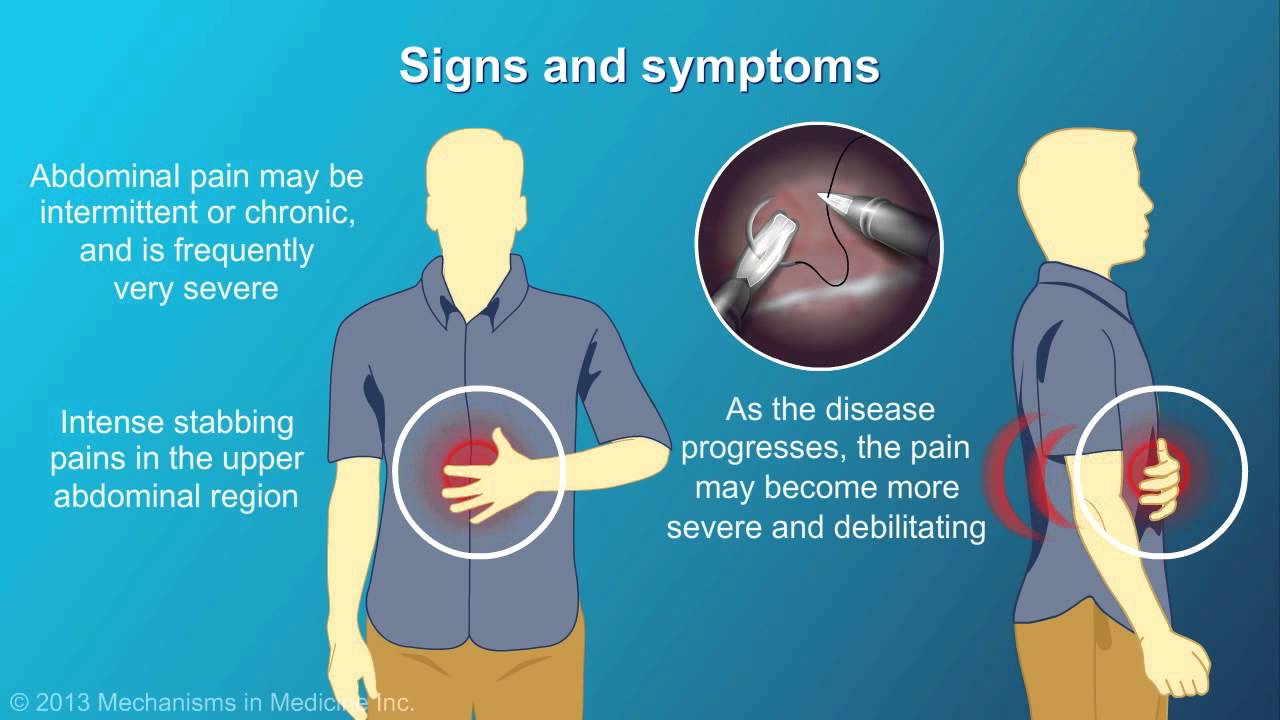
Chronic Pancreatitis Symptoms
The most common symptom of chronic pancreatitis is abdominal pain, which can be severe and debilitating. This pain typically occurs in the upper abdomen and may radiate to the back. It can be constant or episodic, often worsened by eating or drinking, especially fatty foods or alcohol. Other symptoms include weight loss, due to malabsorption of nutrients, and steatorrhea, which is the presence of excess fat in the stools.
Patients with chronic pancreatitis may also experience nausea, vomiting, and bloating. As the disease progresses, it can lead to diabetes mellitus due to the destruction of insulin-producing cells in the pancreas. This results in symptoms like increased thirst, frequent urination, and unexplained weight loss. The chronic inflammation can also lead to the development of pancreatic cysts and an increased risk of pancreatic cancer.
The most common symptom of chronic pancreatitis is abdominal pain which is often chronically intermittent with sharp stabbing pain the abdomen of the stomach since the pancreas is located behind the stomach.
That’s why the pain will radiate to the back. The pain is often triggered by eating foods high in fat. Weight loss is usually experience in advanced stages chronic pancreatitis usually signalling the existence of “pancreatic insufficiency“. Severe cases can lead to developing diabetes.
There is No Cure For Chronic Pancreatitis
Chronic pancreatitis is a progressive disease for which there is currently no cure. The management of chronic pancreatitis focuses on relieving symptoms, managing complications, and slowing the progression of the disease. Lifestyle modifications, such as abstaining from alcohol and smoking, are crucial in managing chronic pancreatitis. Pain management is another critical aspect, often requiring a combination of medications, including enzyme supplements, and sometimes more invasive procedures or surgeries.
Nutritional support is vital to address malabsorption issues. Patients may need a special diet that is low in fat and rich in nutrients, along with vitamin and mineral supplements. Monitoring and managing diabetes if it develops is also important. In some cases, surgical interventions might be necessary to relieve pain, address complications like pseudocysts, or treat associated conditions such as biliary tract disease.
Early diagnosis and treatment can help slow the progression of the disease. Treatment involves avoiding triggers, such as heavy alcohol use, smoking and eating food with very high levels of fat which can slow the progression of chronic pancreatitis. It is always advisable to seek the advice of a registered nutrition specialist who can design a healthy diet to control the symptoms along with multivitamins.
Pancreas Enzyme Replacement Therapy (PERT) Will Become Necessary
Pancreatic digestive enzyme replacement is necessary treatment with prescription medications that act as the substitute for the absence or diminished performance of natural digestive enzymes produced by the pancreas.
Pancreas Enzyme Replacement Therapy (PERT) is often necessary for individuals with chronic pancreatitis, especially when the condition leads to pancreatic exocrine insufficiency. PERT involves taking pancreatic enzyme supplements to aid in the digestion of food. These supplements contain a mixture of digestive enzymes, including lipase, protease, and amylase, which are normally produced by the pancreas.
PERT helps in the proper digestion and absorption of nutrients, thus improving nutritional status and quality of life. The therapy is tailored to each individual, with the dosage adjusted based on the severity of the enzyme insufficiency, diet, and the presence of steatorrhea. Patients on PERT should be monitored regularly to assess the efficacy of the treatment and make necessary adjustments. This therapy is a cornerstone in the management of chronic pancreatitis, as it addresses one of the fundamental problems caused by the disease.
Pancreatic digestive enzyme replacement is necessary treatment with prescription medications that act as the substitute for the absence or diminished performance of natural digestive enzymes produced by the pancreas.
Managing Chronic Pancreatitis
In conclusion, chronic pancreatitis presents a complex and challenging scenario in gastroenterology, with its irreversible impact on both the exocrine and endocrine functions of the pancreas. This disease underscores the intricate relationship between lifestyle choices, genetic predisposition, and the intricate workings of the human body. Key factors like a family history of pancreatic disease, autoimmune conditions, and lifestyle habits like heavy alcohol use and smoking significantly contribute to the onset and progression of chronic pancreatitis. The blockage of pancreatic ducts, often by gallstones, is another critical aspect that necessitates careful examination through diagnostic methods such as CT scans, blood tests, and endoscopy. The resultant malnutrition, abnormalities in glucose management, and fluctuating blood sugar levels are direct consequences of this debilitating condition. Moreover, the role of the immune system in some cases of chronic pancreatitis highlights the complexity of this condition, which often requires a holistic approach in healthcare management.
The management of chronic pancreatitis involves a multifaceted approach, including Pancreas Enzyme Replacement Therapy (PERT) to address pancreatic exocrine insufficiency (EPI), dietary adjustments to manage malnutrition, and interventions to regulate blood sugar levels, such as monitoring glucagon and insulin. In severe cases, surgical options like pancreatectomy may be considered. The importance of early diagnosis cannot be overstated, as it provides a window for mitigating the progressive damage caused by this disease. The potential hereditary nature of pancreatitis also calls for a greater emphasis on family history in the assessment and treatment plan. Overall, the management of chronic pancreatitis is a testament to the advances in gastroenterology, yet it also serves as a reminder of the ongoing challenges in treating complex pancreatic diseases.
Video Describing Nutrition Management For Those With Chronic Pancreatitis
This article is provided for educational awareness only by the Seena Magowitz Foundation For Pancreatic Cancer Research and is not intended to replace professional medical advice. Always consult with your medical providers for medical advice. The article describes the purpose of the pancreas and what causes chronic pancreatitis, its causes, symptoms, and risk factors