Causes of Pancreatic Insufficiency, Risk Factors, Symptoms, and Treatment
On This Page: Pancreatic Insufficiency
Jump To Section
Video Compliments of The National Pancreas Association
Written By Tony Subia
Nov 29, 2021
What Is Exocrine Pancreatic Insufficiency?
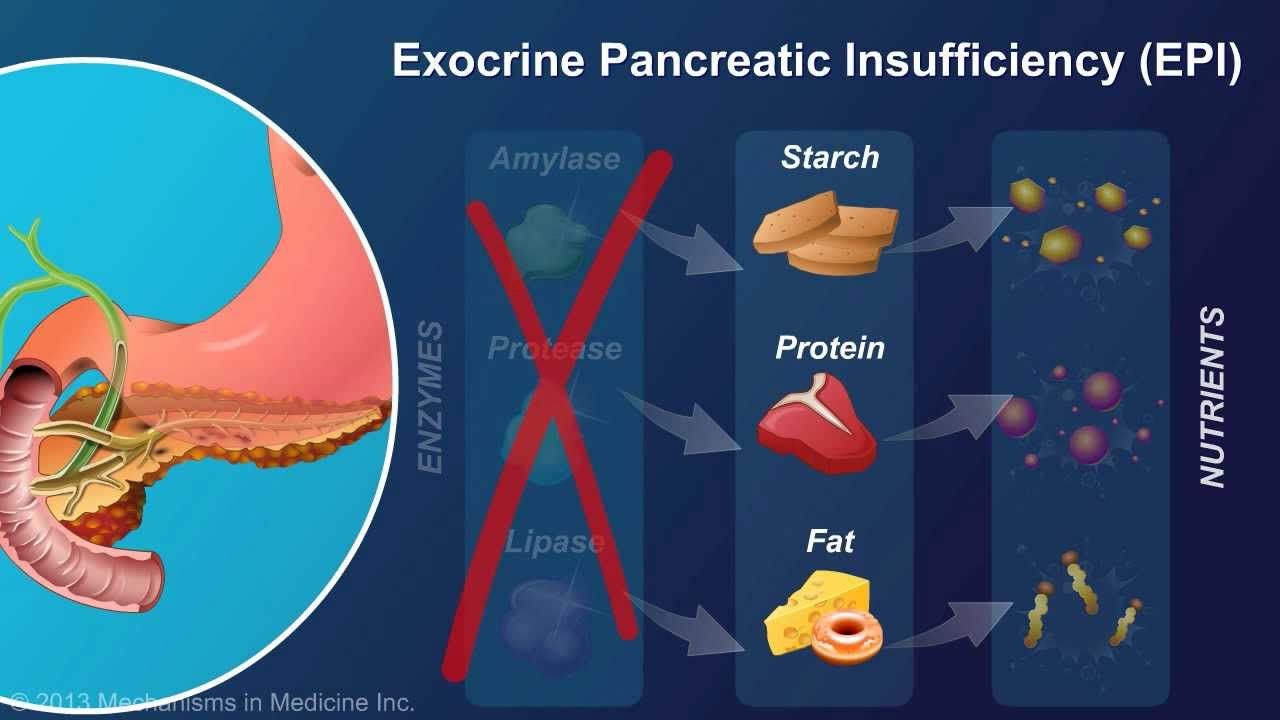
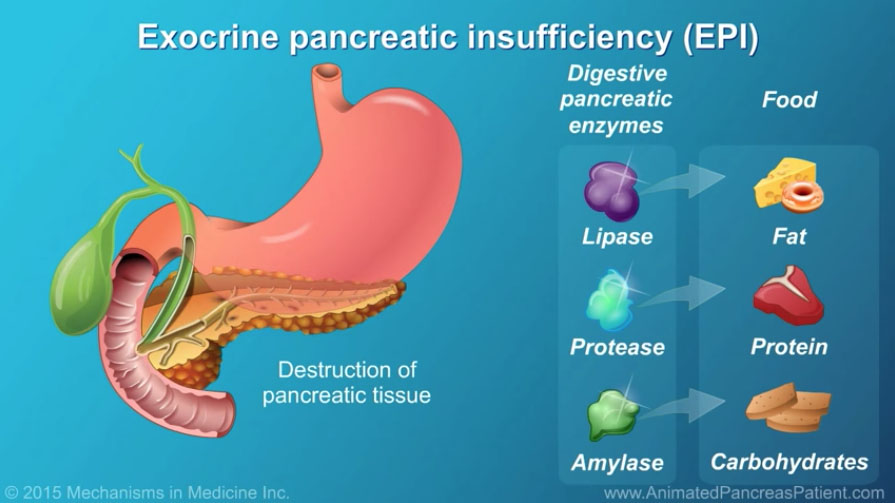
Pancreatic Insufficiency, or exocrine pancreatic insufficiency (EPI), is a condition where the pancreas fails to produce necessary digestive enzymes, leading to significant health issues like malnutrition, weight loss, abdominal pain, and fatigue. This disease can stem from various causes, including chronic pancreatitis, cystic fibrosis, and conditions such as pancreatic cancer. Symptoms like steatorrhea – where undigested fat alters bowel movements – gas, bloating, and unexplained weight loss, are key indicators of this condition. Diagnosis involves a range of tests, including blood tests, fecal elastase measurements, and pancreatic function tests, often conducted in a gastroenterology setting.
Treatment for EPI involves a multi-faceted approach. Pancreatic enzyme replacement therapy is a common method, supplemented by dietary adjustments guided by a dietitian. Managing the condition also includes the intake of fat-soluble vitamins and addressing potential vitamin deficiencies. Additionally, conditions like Shwachman-Diamond syndrome, Crohn’s disease, and other inflammatory bowel diseases are closely monitored due to their impact on pancreatic function. Understanding EPI is crucial not just for those directly affected, but also for healthcare providers, as it requires a comprehensive understanding of digestive tract health, enzyme products, and the overall exocrine function of the pancreas.
The Digestion Process
To completely understand the adverse effects of pancreatic insufficiency, it helps to understand the digestion process. Digestion is a very complex process of converting the food we eat into vital nutrients which the body requires to provide energy and cell repair needed for survival.
Digestion begins in the mouth. As you take your first bite, your salivary glands release saliva. When saliva mixes with food in the chewing process it breaks food into smaller pieces that can be easily swallowed into the throat which passes them to the esophagus which in turn funnels them into the stomach.
The stomach produces stomach enzymes and secretes a strong acid. Together they initialize the process of breaking down food into usable energy form. When the stomach is ready to send the food fragments to the small intestine it sends a message to the pancreas to begin producing and secreting pancreatic digestive enzymes.After food contents are processed in the stomach, they are released into the duodenum which is at the beginning of the small intestine.
The broken-down pieces of food in the stomach is sent to the small intestine in a “semi solid state”. The pancreas then begins to release “inactive digestive enzymes” through the pancreatic duct. It joins with the
bile duct which is a digestive solution that helps digest fats.
Bile is produced by the liver and stored in the gallbladder. As fatty foods enter the small intestine, the gallbladder squeezes bile into the small intestine through the bile ducts.
Digestive Enzymes Produced By The Pancreas
> Amylease. It breaks carbohydrates
> Lipase. It breaks down fats.
> Proteease and Elastase. Breaks down proteins.
What Causes Pancreatic Insufficiency?
There can be several causes of pancreatic insufficiency. Any condition that can lead to damage of the pancreas which prevents its production of efficient digestive enzymes or blocks the release of digestive enzymes into the small intestine can cause pancreatic insufficiency.
Cystic fibrosis is an inherited genetic disease meaning a child is born with cystic fibrosis. It is a progressive disease which causes a buildup of sticky mucus which blocks the liver bile ducts. This causes inflammation and scarring of the liver which produces bile. The blockage of the bile duct prevents bile from reaching the small intestine where it helps to digest fats.
Chronic pancreatitis is caused a long term, intensely serious inflammation of the pancreas that recurs. It leads to an irreversible severe destruction of the pancreas.which prevents the ability of the pancreas to produce digestive enzymes which results in pancreatic insufficiency.
Pancreatic cancer often results in exocrine pancreatic insufficiency (EPI). In fact studies show that pancreatic cancer patients taking pancreatic enzyme replacement therapy (PERT) live longer compared to those diagnosed by other causes beside pancreatic cancer. It is interested to note that pancreatic insufficiency does not cause pancreatic cancer but is sometimes a symptom of pancreatic cancer.
Other causes of pancreatic insufficiency include the following:
> A severe case of acute pancreatitis primarily caused when gallstones block the bile duct preventing pancreatic enzymes from reaching the small intestine. In those cases , enzymes become prematurely activated while still in the pancreas. This results in the “activated enzymes” to actually begin digesting the pancreas itself causing severe and extremely painful inflammation of the pancreas.
> Surgical removal of the pancreas. Of course it is a cause since there would be no pancreas to produce digestive enzymes.
> Celiac disease is a type of autoimmune disease where the immune system has adverse reaction to gluten. Exposure to gluten can cause inflammation that can gradually damage the small intestine. The damage can restrict the absorption of molecules of nutrients through the walls of the small intestine into the bloodstream.
> Tumors. Whether they are benign or malignant can block the the release of digestive enzymes into the small intestine.
> Autoimmune pancreatitis where chronic inflammation of the pancreas is caused by the body’s own immune system attacking the pancreas.
What Are The Symptoms of Pancreatic Insufficiency?
> Steatorrhea. Steatorrhea is the most common sign of pancreatic insufficiency. People that have
pancreatic insufficiency typically cannot absorb all the fat they eat. Undigested fat which passes
through the digestive system leads to stools that float, are greasy, foul smelling, and hard to flush.
> Gas and bloating can cause stomach pain that could radiate to the back especially after eating
> Stomach pain in the upper abdomen area that often radiates to the back especially after eating.
> Nausea and vomiting.
> Unexplained weight loss. The result of malnutrition.
> Diarrhea.
> Lack of energy, fatigue, and dizziness. The result of malnutrition.
Compliments of The National Pancreas Foundation
Most often, exocrine pancretic insufficiency (EPI) is a lifelong condition, although in some limited situations it can be repaired. “Pancreatic Enzyme Replacement Therapy” (PERT) is necessary treatment with prescription medications containing enzymes that act as the substitute for the missing or diminished performance of natural pancreas- produced digestive enzymes.
> Replacement enzymes include lipase, protease and amylase which are combined in pill form and must be taken with every first bite of a full meal or snack. A second dose could be taken at the end of main meals. Waiting until after you eat is too late to have a positive effect. Doses come in various unit values that likely requires a bit of trial and error to arrive at the most desirable dosage. Speak with your physician for recommendations after a diagnosis of pancreatic insufficiency.
> A well-balanced diet. A good diet for pancreatic insufficiency includes the following nutritional foods:Fruits, vegetables, lean meats, fish, skinless poultry, beans, lentils, low fat dairy, sweet potatoes, avocados, blue berries, black berries, natural nuts (particularly pecans and almonds), and low-fat dairy. Polyunsaturated fats are okay including olive, canola, and peanut oils. Surprisingly cheeses and dark chocolates are fine in moderation.
If you’ve been diagnosed with pancreatic insufficiency, ask your doctor to recommend an expert nutritionist to design ideal diets for meals and snacks.
> Foods to avoid. Avoid foods with high saturated fats including butter, ice cream, chicken skin, turkey skin, pork skins, fatty cuts of meat, and pastries. Also avoid trans fats, hydrogenated oil, tropical oils like coconut and palm oils,fried food, creamy style foods and packaged foods. Always avoid alcoholic drinks.
> Eat smaller meals. Instead of three large main meals, try 4 to 6 smaller meals each day. Try and include a healthy protein with each meal. Also try and limit consumption of total fat content of 30 to 50 grams per day. Snacks including dark chocolates, fruits, low-fat yogurts, and jellos are great choices as snacks.
> Stay well hydrated with water. and avoid high-calorie beverages.
> Keep low triglyceride levels. Talk to your doctor about the prescription drug “Fenofibrate”.
Take fat soluble supplements. Vitamins D, A, E, and K. Take Vitamin B-12 for increase energy.
Concluding Thoughts on Pancreatic Insufficiency
In summary, exocrine pancreatic insufficiency (EPI) is a complex gastrointestinal disorder that primarily involves the malabsorption of nutrients due to insufficient enzyme production by the pancreas. Understanding the cause of EPI is crucial, as it can stem from a variety of pancreatic diseases, including chronic inflammation or damage to the pancreas. The prevalence of EPI is notably associated with conditions like type 2 diabetes and osteoporosis, underscoring the importance of early detection and management.
Symptoms of EPI are diverse, ranging from maldigestion to more specific signs like changes in bowel movements detected through a fecal fat test. Tools like endoscopic ultrasound and tests measuring elastase-1 levels are vital in diagnosing EPI, offering insights into both exocrine and endocrine functions of the pancreas. Additionally, secretin stimulation tests can help evaluate pancreatic secretion, providing a more comprehensive view of pancreatic health.
Managing EPI often involves addressing its side effects and ensuring adequate intake of essential nutrients, including vitamins A and other fat-soluble vitamins. It’s important for patients and healthcare providers to be aware of the intricacies of EPI, including its gastrointestinal, gastric, and malabsorption aspects, to effectively manage this condition and improve quality of life for those affected. As our understanding of pancreatic diseases continues to evolve, so too will our strategies for combating conditions like EPI, offering hope and improved outcomes for those impacted by this challenging disorder.
Compliments of The National Pancreas Association
Information Sources
Cleveland Clinic
National Center of Biotechnology
National Pancreas Foundation
CREON
The above information about exocrine pancreatic insufficiency, its symptoms, causes and treatment are provided as educational information only. It is not intended as medical advice which can only be provided by physicians. It is not intended as a substitute for professional expert medical opinion, advice, or diagnosis. If you have symptoms consult with your physician for medical direction.