10-year survival rate after whipple surgery
10-year survival rate after whipple surgery
Whipple Surgery For Malignant Tumors in the Pancreas
As it relates to pancreatic cancer, the Whipple Surgery Procedure is performed when the tumor is only within the pancreas and has not metastasized (spread to other organs or tissue). Once the cancer has spread, surgical removal of the primary malignant tumor from the pancreas will not benefit the patient. Once the cancer has spread to lymph nodes, blood vessels, or other organs, pancreatic cancer is difficult to treat and survival is remote.
This is why early discovery is crucial. You should be very cognizant of risk factors and symptoms of pancreatic cancer. People must be diligent and vigil. Only 9% of cases are diagnosed while the tumor is confined to the pancreas. When detected prior to metastasis, the 5-year survival rate is 26% versus only 2.3% when discovered at very distant stages. The overall survival rate is about 6% when diagnosed at all stages.
What is Whipple Surgery?
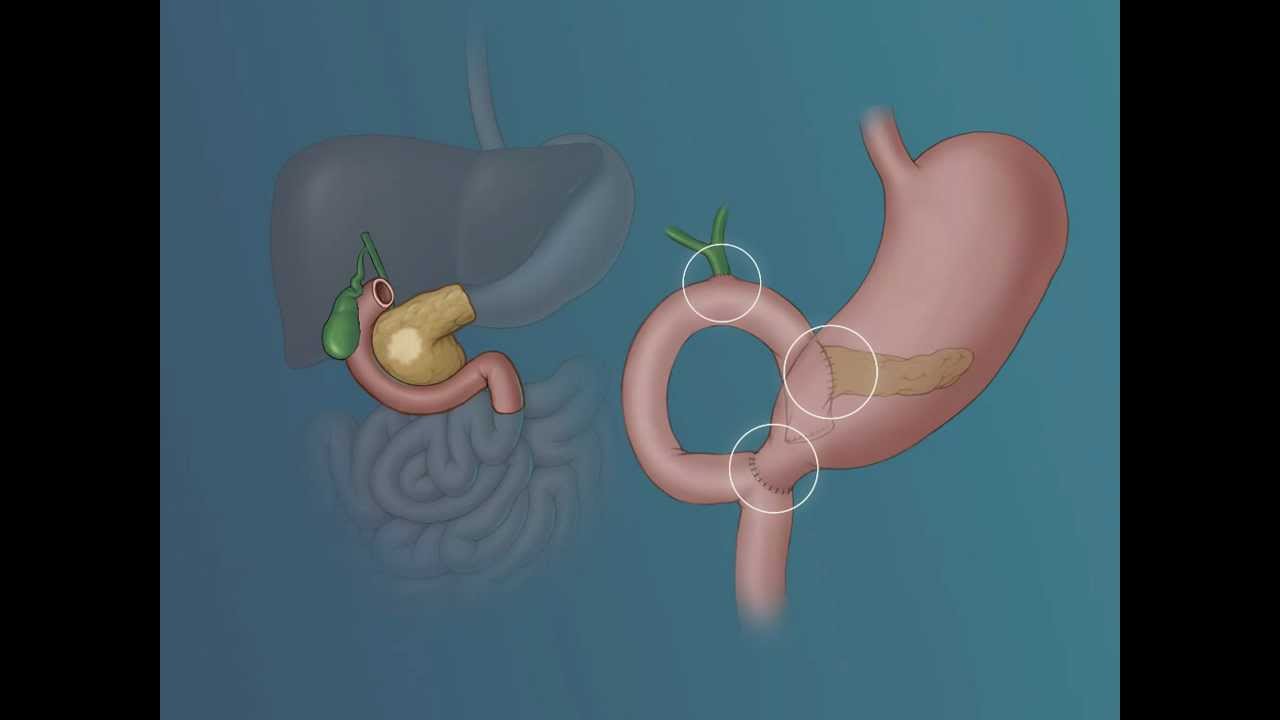
Whipple surgery (or Whipple procedure) is the surgical option when pancreatic cancer is found in the head of the pancreas. It involves removal of the pancreas head, most of the duodenum (small intestine), a portion of the bile duct, gallbladder, part of the jejunum and lymph nodes located near the pancreas. Sometimes a portion of the stomach may also be removed.
After surgical removal, the remaining balance of the pancreas and bile duct is attached to the small intestine permitting bile from the liver to continue entering the small intestine. It allows the remaining parts of the pancreas, stomach and intestines to sustain the digestive process.
Well-informed decisions should always be based upon the advice of physicians, surgeons and other medical experts. Studies show that surgical skill, experience and volume of successful Whipple Surgeries performed by the surgeon and hospital will have a greater success rate. Careful research by the patient is crucial.
Risk During Whipple Surgery
The Whipple Operation is a major surgery with degrees of variable risk. The extreme risk is not surviving the surgery. In the 1960s and 70s, about 25% of patients did not survive the operation. Today, with medical advancement and experience, it is a much safer operation with a significant reduction in mortality rates during surgery.
A study from Johns Hopkins and Memorial Sloan Kettering shows a correlation of survival rate versus the experience of both hospital and surgeon. Hospitals that perform a high number of Whipple operations experience a death rate of less than 4%. Those hospitals that perform few Whipple surgeries may experience a significantly higher death rate. A study by The New England Journal of Medicine found operative mortality rates to be four times higher (16.3 %vs. 3.8%) at low-volume (averaging less than one per year) hospitals versus high-volume (16 or more per year) hospitals.
Risks After Whipple Surgery
After Whipple surgery, the patient can expect a hospital stay of 10 to 14 days for recovery and protection against post-surgery risks and complications. Among immediate risks are infection, bleeding. leaking of digestive enzymes, pancreas inflammation and possibility of other organ failure including the heart, liver and kidneys.
One of the purposes of the pancreas is producing digestive enzymes. Since pancreatic tissue is removed during surgery, diminished enzyme production could cause digestive problems. Long-term use of an oral enzyme supplementation may be necessary. Eating habits typically have to change with smaller meals and in between snacks.
It takes several days after surgery for bowel functions to return. Intravenous feeding nutrition is followed by progressive stages of diet from liquids to an eventual regular diet as normal function gradually returns. There is about a 25% chance the stomach may be temporarily paralyzed. The surgeon may place a feeding tube into the intestine at time of surgery where it will remain until normal stomach functions return.
Developing diabetes is a risk. One of the roles of the pancreas is producing insulin to control blood sugar. Since certain pancreas tissue is removed during surgery, the remaining parts of the pancreas may not produce enough insulin creating the risk of developing diabetes. Patients that have no diabetic history have a low probability of developing diabetes. If diabetes exists, it can become more severe after surgery.
More Whipple Procedure Information
Before and After Surgery Illustration
Whipple Procedure: WebMD