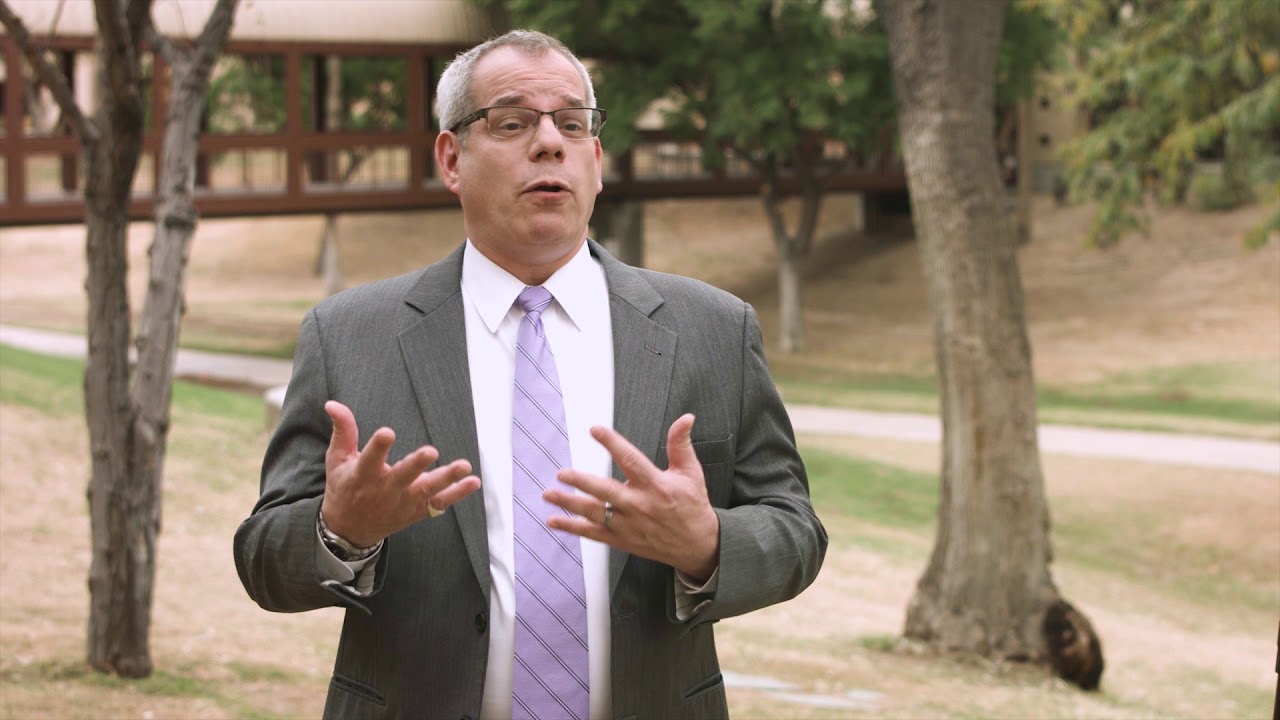
When the Oncologist Becomes a Patient: Dr. Michael Gordon’s Story
Written By: Julia Brabant
June 2023
Date of Diagnosis: May 2021
Current Status: No Sign of Active Cancer
It’s impossible to prepare oneself for a pancreatic cancer diagnosis, but as a medical oncologist and the Chief Medical Officer at the HonorHealth Research Institute in Scottsdale, Arizona, Dr. Michael Gordon knew more than most about what to expect after his own. Now, several years post-surgery, he shows no evidence of disease, but he does offer a unique perspective as someone who has not only treated pancreatic cancer but survived it.
In his role at HonorHealth, Dr. Gordon oversees all research activities including within the Division of Cancer Research, helping expand patient access to innovative, cutting-edge clinical trials and treatment methods. As an oncologist with decades in practice, Dr. Gordon also knew better than to ignore even subtle health symptoms, so when he started experiencing uncharacteristic itchiness and seeing changes to the color of his stool and urine, he sought treatment from an internist.
The internist determined Dr. Gordon’s bilirubin and liver enzyme levels were elevated and conducted a series of tests, including a CT scan, an endoscopic ultrasound and an ERCP. Tests revealed a large cystic mass in the head of the pancreas with intraductal papillary mucinous neoplasms, or IPMN. IPMN are cysts in the pancreas that are initially benign but have the potential to progress into cancerous tumors.
Dr. Gordon’s medical team used a technique called pancreatic duct brushing to make a diagnosis of adenocarcinoma. PET and MRI scans showed that his cancer had not progressed outside the pancreas and was likely “resectable,” or eligible for surgical removal.
Before he could have surgery, though, Dr. Gordon’s care team set to work shrinking the tumor by administering neoadjuvant therapy. This type of therapy seeks to help prepare a patient for surgery or another primary treatment. He underwent four cycles of chemotherapy and five weeks of radiation, and in November 2021, he traveled to Milwaukee, Wisconsin, to have a Whipple procedure.
Dr. Douglas B. Evans of Froedtert & the Medical College of Wisconsin performed the Whipple surgery, after which pathologists determined there was no more evidence of disease. Dr. Gordon took some time to recover from the intensive procedure before beginning two more months of maintenance chemotherapy to help lessen the chances of the cancer coming back.
Now, he has health assessments every three months to monitor his condition. If everything looks good by the two-year anniversary of his Whipple procedure, he may start waiting six months between follow-up visits. Like many Whipple patients, Dr. Gordon has had to tweak his diet and take CREON, which helps with digestion, with most meals. While he never developed diabetes, which happens to some pancreatic cancer patients, Dr. Gordon does take Metformin, which studies suggest may lower the risk of pancreatic cancer for some patients.
Having been identified as having a high-risk gene for the development of cancer, Dr. Gordon remains under surveillance for other cancers.
Seeking – and Supplying – Answers
Many people with pancreatic cancer have no family history of the condition, and Dr. Gordon is among them. However, he did have genetic testing done to see if he had gene mutations that heightened his chances of getting cancer, and the tests showed he had a pathogenic ATM mutation, which may increase the chances of pancreatic and prostate cancers.
While seeking answers about what might have contributed to his own cancer risk, Dr. Gordon returned to full-time work. When he’d anticipated taking a leave of absence to have surgery, he’d messaged his own cancer patients, many of whom had noticed his hair and weight loss. He wanted to ease their concerns, and he also hoped his own story might give them hope while they worked through their own diagnoses.
“Having cancer does give you novel insight about what it’s like to a be a patient with these issues,” Dr. Gordon said. “You develop a unique sense of empathy when it comes to things like the cognitive effects of chemo; experiences with neuropathy…it can help patients to know that the person taking care of them shared their experiences.”
Dr. Gordon noted that while no two people with metastatic diseases have identical experiences, many do go through similar struggles and often don’t have adequate time to prepare for the decision-making process that follows a cancer diagnosis.
For this reason, he’s a strong advocate for taking advantage of support groups, pancreatic cancer organizations and other resources that unite people facing similar health struggles. Dr. Gordon also says that while he does not treat pancreatic cancer patients directly, for him, getting back to work within the greater cancer community was part of the healing process.
“My role as an oncologist prepared me better for the highs, lows and complexities of being a cancer patient, but I had a whole team treating me,” he said. “I hope my own patients see me as a success story…they’re a big part of me coming back to doing what I love.”
Dr. Michael Gordon continues to oversee research operations at the HonorHealth Research Institute and undergo regular monitoring of his condition as of June 2023.