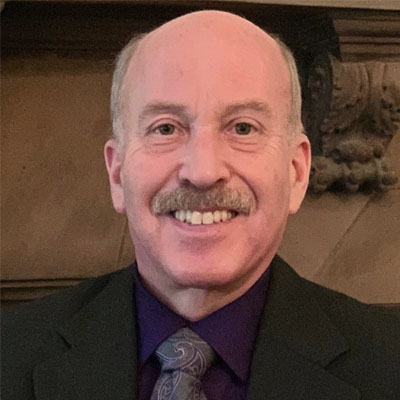
STEVE MERLIN: PANCREATIC CANCER SURVIVOR
Written By: Julia Brabant
August 2023
Date of Diagnosis: June 2012
Current Status: No Sign of Active Cancer
Steven Merlin: an 11-Year Pancreatic Cancer Survivor Makes a Strong Case for Second Opinions, Clinical Trials & Mentorship
Steven Merlin’s doctor called him the “picture of health” when he scheduled a visit for mild symptoms in 2012, and it wasn’t until he sought several more opinions that Steven learned he had pancreatic cancer. Now, 11 years later, Steven uses the knowledge he gained through both his personal experiences and his career as a medical researcher to guide other people with cancer as a patient mentor.
Initially, Steven’s symptoms were mild. He noticed his urine had darkened, but he wasn’t a big water drinker, so he started hydrating more. When that didn’t help, he went to his primary care physician, who said he was, by all accounts, in optimal health. Aside from the urine issue, Steven wasn’t surprised – he’d always eaten well, and he was fit, often riding his bike a couple hundred miles in a week.
When Steven’s symptoms continued, he went to a different PCP for a second opinion. That doctor concurred with the first one but told him to come back at the end of the week if he didn’t see improvement. He went home, but gastritis, or stomach inflammation, soon set in.
Steven asked his doctor to run blood tests. As a medical technologist with a background in immunology and cancer, stem cell and biomedical research, he knew how to interpret them. While awaiting the results, jaundice, or yellowing of Steven’s skin and eyes, became noticeable.
He thought the cause might be a gallbladder issue. His dad had gallbladder disease at the same age Steven was now, so he returned to the doctor for more testing. A sonogram didn’t reveal anything out of the ordinary, so his doctor sent him to a gastroenterologist for more tests.
After reviewing test results, the GI doctor recommended Steven have an endoscopic ultrasound, which helps doctors view the inside of the digestive tract. The doctor then told Steven he had good news and bad news.
The bad news: They’d encountered bile duct compression when installing a stent, suggesting a large mass that was likely cancerous.
The good news: Steven was eligible for the Whipple procedure, and the hospital’s chief of surgery for hepatobiliary diseases was able insert a stent the following day and do the Whipple procedure a day later – on a Saturday.
Caught off-guard, Steven asked doctors if they could delay it to the following Monday to give him to time to line up help at home and otherwise prepare for the complex procedure. His surgeon agreed on doing the surgery two days later.
The urgency was due to the severity of Steven’s case – he had an aggressive tumor in proximity to the portal vein. He was in ideal physical condition, making him a good candidate for a Whipple. He had the Whipple surgery June 18, 2012.
It wasn’t until after a post-surgical CT scan that Steven learned that his cancer, a rare form known as acinar cell carcinoma, had metastasized to his liver. The metastasis hadn’t been detectable during the initial diagnostic scan but progressed rapidly enough to become so within a matter of two weeks. Because the cancer had metastasized, doctors determined he was Stage 4 – with Stage 4 patients typically not being eligible for the Whipple procedure Steven had just had.
The tumor board at the hospital recommended he begin palliative chemotherapy using Gemzar to treat the metastasis. After three months, he found out he was part of the 10% of the population that don’t produce the liver enzyme needed to break down Gemzar, rendering those three months of chemo ineffective.
At the initial meeting with his oncologist, Steven expressed his goal of long-term survival and willingness to do aggressive chemotherapy with FOLFIRINOX and radiation, as it was determined to be of added benefit. After reviewing earlier notes on the tumor board’s decision of recommending palliative care, he was surprised his oncologist hadn’t made more of an argument to the board for aggressive chemo given his successful recovery from the Whipple, his relatively young age and his otherwise excellent physical condition.
“I thought he’d stand up for me and say I was a unique case,” Steven said. “At the time, I didn’t know if appealing to the tumor board might be an option.”
This time, Steven was prepared to advocate for the more aggressive treatment he initially indicated he was willing to take.
His oncologist agreed to the request of more aggressive treatment using FOLFIRINOX. The new drug was effective, and Steven’s tumor started shrinking significantly. While on this regimen, he saw a geneticist, and genetic tests revealed he had the BRCA2 gene mutation.
His doctor said this was good news, meaning he had a “targetable mutation.” As a result, he was a candidate for a clinical trial. The clinical trial was a targeted therapy that involved taking a PARP inhibitor, a type of cancer drug that was, at the time, only available to people with ovarian or breast cancers.
Steven wound up being the first person from the United States to join this particular multi-national clinical trial – and he remains on it today, making him the longest pancreatic patient in the world still benefiting from the drug. His particular drug has not yet received FDA approval, so he was able to obtain it free of charge because he qualifies for “compassionate use” and continues to take it because his gene mutation puts him at an elevated risk for a new primary pancreatic cancer as well as prostate and male breast cancers. To date, he’s had only a minor side effect of anemia and no recurrence of cancer since enrolling in the trial in 2014.
The Patient Becomes a Mentor
These days, Steven relies on his knowledge of the medical field and his experiences as a patient to guide and mentor other patients with pancreatic cancer. He’s also teamed up with a number of research and advocacy organizations, including the Pancreatic Cancer Action Network, LetsWinPC.org, Hematology/Oncology Pharmacy Association (HOPA), American Society of Clinical Oncology (ASCO), the non-profit Medical Research Organization ECOG-ACRIN and the Multinational Association of Supportive Care in Cancer (MASCC) as a patient advocate. He is also active in a number of Pancreatic Cancer Support Groups.
While each mentorship is unique, there are certain things Steven encourages everyone with pancreatic cancer to do.
First, he urges patients to select a major, comprehensive cancer center that has an established, proven high-volume program focusing on pancreatic cancer or hepatobiliary diseases.
“All pancreatic cancer oncologists are GI specialists, but not all GI specialists are pancreatic cancer oncologists,” he said “At major cancer centers, they employ a multidisciplinary approach, and that’s where you’re going to find pancreatic specialists with a higher level of expertise in treating pancreatic cancers.”
He also encourages people with pancreatic cancer to focus on what they can control, feel comfortable asking questions, and if their goal is long-term survival, have the strongest possible treatment their bodies can tolerate.
“All it takes is one cancer cell left behind,” he said. “If your immune system weakens, that one cell can replicate, and it often is more aggressive the second time around.”
Keeping the immune system strong and exercising to build stamina will help in tolerating strong treatments and getting through them in the first place, Steven says.For this reason, he urges the patients he mentors to stay active and healthy. He also believes that the more information a patient has about his or her condition and options, the easier it is to make educated decisions about what steps to take next.
For example, he believes more people need to understand the difference between the “NED” and MRD” acronyms. While “NED” means “no evidence of disease,” “MRD” means “minimal residual disease,” and treatment options vary based on the objective of achieving NED where MRD can still exist, or going further to eliminate it.
“If a patient has MRD, more chemo may be necessary to eliminate the cancerous cells that remain,” he said. “This cancer has such a high propensity to come back, so you don’t want to throw caution to the wind when there are still may be cancerous cells in the body.”
Steven also empowers patients whose medical teams recommend palliative care to challenge that recommendation when they are younger, physically fit and have no significant co-morbidities, and patients whose teams recommend clinical trials to seriously consider them – especially patients who received late-stage diagnoses.
“Clinical trials aren’t just for people with certain biomarkers,” Steven said. “Some of them target cellular pathways and other areas that can help stop cancer in its tracks. Some of them also involve taking pills, which can be a lot easier on the body than IV infusions.”
Steven also recommends that people with pancreatic cancer compile a set of medical records, including bloodwork and radiology and pathology reports, and scan them onto a hard drive for later copying to a compact disc, printed out in a binder, or both. Having those records on hand can help eliminate avoidable delays, especially in obtaining a second opinion or applying for a clinical trial, and help ensure that everyone who treats a patient has all the information they need to do so.
Steven also urges oncologists to consider the entirety of a patient’s condition before deciding how to move forward.
“It’s important to consider a patient’s physical, mental and emotional health when deciding what treatment to recommend,” he said. “Don’t write a particular treatment off without considering whether someone is physically, mentally and emotionally strong enough to handle it.”
Steven also cautions pancreatic cancer survivors against going too long between scans, even though many doctors space them out further, or phase them out entirely, once someone hits that five-year mark.
“After five years, they told me I don’t need frequent scans, but I still have them not just once a year, but twice,” Steven said. “It’s a small sacrifice to make for something that could save your life.”
Steven Merlin has shown no sign of cancer since completing treatment with FOLFIRINOX in September 2014.