Early Detection and Tailored Treatment Made a Difference for 7-Year Pancreatic Cancer Survivor & Veteran Duane “Dewey” Hill
Contributing Writer
Julia Brabant
October 1, 2024
Diagnosed: September 2017
Current Status: Currently cancer free
Duane “Dewey” Hill’s experience with pancreatic cancer highlights the difference an early diagnosis and skilled medical care can make. While no journey with pancreatic cancer is “easy,” Dewey’s path was less arduous thanks to early detection, prompt action and the quality of care he received throughout his treatment.
The first clue that something was amiss with his health came in September 2017, when Dewey, a veteran from Pleasant Prairie, Wisconsin, noticed his urine taking on a dark tone. He didn’t think much of it initially, but when he started vomiting after eating and no one who had the same dinner as him did the same, he started to wonder. Soon after, his daughter remarked that his eyes were turning yellow, prompting Dewey to visit a nearby VA hospital where they promptly diagnosed him with pancreatic cancer.
The doctors at the hospital performed an ERCP and identified multiple spots on Dewey’s pancreas, leading to a Stage 2 diagnosis. It turned out one of the Dewey’s masses was blocking his bile duct, which led to the abdominal problems and caused his jaundice.
“It was a blessing in disguise,” he said, of the blockage. “If it wasn’t for the bile backing up, I might have been dead by now.”
Dewey’s medical team installed a stent to relieve his symptoms and had him meet with Dr. Susan Tsai, a surgical oncologist and one of the nation’s premier pancreatic cancer specialists. Dr. Tsai had worked with veterans with cancer for more than a decade through a longstanding partnership between the Medical College of Wisconsin and the Clement J. Zablocki Veterans’ Administration Medical Center.
Research suggests that some veterans face an elevated risk of pancreatic cancer due to exposure to burn pits, radiation and other toxic substances during their service. Some veterans also develop cancer due to Type 2 diabetes stemming from military service.
The doctors Dewey initially saw suggested he have surgery. However, Dewey wanted to know more about alternative options so he wouldn’t become dependent on insulin and CREON, a digestive enzyme many people with pancreatic cancer take with meals post-surgery, for the rest of his life.
Dr. Tsai suggested a combination of chemo and radiation as an alternative. Dewey agreed to the regimen, starting eight rounds of chemotherapy using FOLFIRINOX in December 2017. Originally, his team recommended four rounds of chemo, but because of how well his body responded, they decided to move forward with eight.
While FOLFIRINOX is known to produce some unsavory side effects, Dewey completed his treatments relatively unscathed, seeing minimal side effects like lethargy and an unidentifiable “thumping” sensation in his chest along the way. He did, however, develop several infections in his stent, leading doctors to question whether his body was becoming immune to the antibiotics.
After completing the eight rounds of chemotherapy, Dewey began radiation. Because of the repeat infections and Dewey’s hesitation to have a full pancreaticoduodenectomy, Dr. Tsai suggested he consider a third option; a biliary duct bypass. The procedure involves rerouting the biliary flow in patients with blocked bile ducts.
Dewey underwent the procedure in April 2019, and it went really well.
“Dr. Tsai is awesome,” Dewey said of his surgeon. “I had no complications whatsoever.”
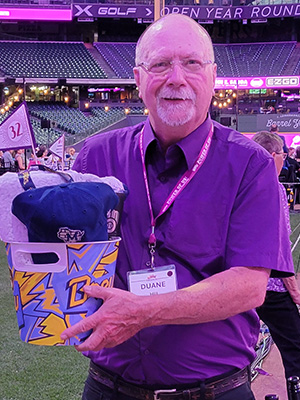
In the aftermath, Dewey had regular checkups to assess his condition, seeing his doctor at first every three months, and then every six months and now once a year. He’s also spent some time with other people facing similar health issues, attending the Seena Magowitz Foundation’s Power of Us fundraiser in Milwaukee in 2024 and hearing from other patients about their own journeys and success stories. Foundation Founder and CEO Roger Magowitz, also a veteran, has a vested interest in veteran health and how pancreatic cancer may disproportionately impact members of this community.
He hopes his story inspires others not to ignore seemingly minor health issues, urging them to seek medical attention at the first sign of something amiss.
“At the first sign of anything, go get checked out,” he said. “If you catch it as early as you can, your chances of survival become much better.”
Dewey also said that his lifestyle is relatively similar to that which he enjoyed before his diagnosis, and that he hasn’t had to make any major lifestyle or dietary changes in the time since his surgery. He did, say, though, that he’s become mellower since his pancreatic cancer diagnosis.