Written By: Julia Brabant
June 2023
Date of Diagnosis: June 27, 2015
Current Status: No Active Cancer
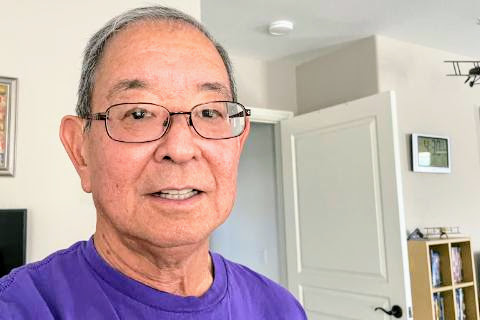
Told He Had No Options, Tom Arai Is Now an 8-Year Pancreatic Cancer Survivor
When doctors diagnosed Yorba Linda, California’s Tom Arai with Stage 4 pancreatic cancer in 2015, the only viable treatment option was a clinical trial involving chemotherapy and an experimental drug. Now, eight years and two clinical trials later, he’s living an active, healthy lifestyle – and has recently signed on to participate in an upcoming pancreatic cancer research effort in collaboration with the U.S. Department of Defense.
Before his diagnosis, Tom, an avid cyclist, was generally healthy and never had any hospital stays or major health concerns. He was prediabetic, though, and was getting treatment for high blood pressure. Still, he was feeling pretty healthy overall when, during a 2015 European River cruise with his wife, Toni, he started having mild abdominal pain and a very low-grade back pain when sleeping.
Tom, who was typically a very light drinker, thought maybe he was overindulging in food or drink during the cruise. He initially thought he had an ulcer.
When he got home, Tom went to see his primary care provider. The doctor recommended he take antacids. When that didn’t work, the doctor advised him to take a prescription medication. When that didn’t work, Tom’s doctor ordered a CT scan, which revealed a suspicious mass. She referred to him to a nearby hospital, where doctors determined Tom had Stage 4 pancreatic cancer that had metastasized to his lungs and liver. Given the progression of Tom’s cancer, doctors said surgery wasn’t an option and there wasn’t much they could do.
At that point, Tom and his wife asked for a referral to an oncologist. They got an appointment with Dr. Tara Seery, a gastrointestinal oncologist at UC Irvine Medical Center. She had just signed on to participate in a Stage 2 clinical trial involving a drug called “PEG20,” and felt that Tom would be a good candidate for the clinical trial.
Given in injection form, the drug may improve the effectiveness of chemotherapy by helping break down the “stroma,” or the material surrounding cancerous tumors, allowing the medicine to target the actual tumors more effectively. Over a 15-month span, Tom had a total of 28 chemotherapy sessions using PEG20.
Tom then began adjuvant therapy, which seeks to help prevent cancer from coming back, using a drug called Xeloda, or Capecitabine. He didn’t tolerate the new drug especially well. However, doctors had identified that Tom had a BRCA gene mutation. Because he had the mutation, and because he had used a specific combination of chemotherapy drugs in past treatments, he became a candidate for another clinical trial.
The new clinical trial, in its third phase, involved a drug called Lynparza. The drug was already FDA-approved for use in patients with cervical cancer, but evidence suggested it could be a viable treatment option for individuals who had the BRCA gene and had gone through metal-based chemo, too.
Now, six-and-a-half years later, Tom still takes Lynparza. While he’d cut way down on biking for a period, he started picking it back up, and he also incorporated regular walks into his schedule when he couldn’t, or didn’t feel up to, getting on the bike.
For the most part, Tom tolerates his ongoing treatment well. He has some neuropathy in his fingertips and on the soles of his feet, and he recently had deep vein thrombosis, which occurs when a blood clot forms in one of the body’s deep veins.
Back in 2016, one of Tom’s follow-up tests showed a spot on his lungs. Because it was too small to biopsy, doctors targeted it using hydros radiation and ultimately determined it was not a cancer recurrence.
“When I was told I had no detectable cancer, my primary care physician said I needed to give back,” Tom said.
Because he’d responded so well to his treatments, his doctor asked if he’d mind talking to other patients to offer insight and support. He agreed, and before long, he was an active participant in a UC Irvine support group that grew rapidly until the onset of the COVID-19 pandemic put a stop to in-person events.
Alongside another survivor, Tom started a weekly Zoom support group for pancreatic cancer patients and survivors who could no longer meet in person. The group still meets today and welcomes referrals from his oncologist, medical centers, Zoom participants and other sources.
Tom is also set to participate in a peer-reviewed research effort in collaboration with the Pancreatic Cancer Research Program (PCARP) at the U.S. Department of Defense. The DoD has an annual budget it dedicates to pancreatic cancer research to help veterans and others battling the disease. This involves doctors, researchers and consumer reviewers evaluating pancreatic cancer research proposals and determining which ones to fund.
“This is something that excites me,” Tom said. “There’s a direct correlation between this effort and future treatment options for patients.”
Tom knows he is very fortunate to be an 8-year survivor and devotes his attention to helping other survivors through programs such as PCARP and other efforts that help pancreatic cancer survivors.
“When told I had Stage 4 metastatic cancer and I found out that the five year survival rate was less than 3%, I didn’t dwell on that,” Tom said. “I choose to focus on one day at a time.”


